Pre-Implantation Genetic Diagnosis (PGD) is an analysis performed as part of IVF programs
before transferring embryos into the uterine cavity. This is a highly accurate study that allows for the identification of hereditary deviations and pathologies. Due to PGD analysis, it is possible to select the most viable and healthy embryos, which reduces the probability of having children with congenital anomalies and hereditary diseases.
Furthermore, PGD of the embryo during IVF makes it possible to minimize the risks of
miscarriages. This analysis is considered one of the most sought-after methods in reproductive medicine.
• PGT-A (Pre-implantation Genetic Testing for Aneuploidy)
• PGT-SR (Pre-implantation Genetic Testing for Structural Rearrangements)
• PGT-M (Pre-implantation Genetic Testing for Monogenic/Single Gene Defects)
PGT-A screening is conducted to diagnose embryos for the presence or absence of chromosomal anomalies. The most common pathology is trisomy (e.g., Down syndrome). Defects in the structure or number of chromosomes cause the development of severe defects and congenital anomalies, including changes in facial features or typical body constitution.
PGT-SR screening is carried out to identify structural chromosomal rearrangements. These are
the cause of various mutations, which can result in the birth of an affected child. This analysis is often performed for couples who are carriers of balanced translocations.
PGT-M screening is performed to identify the risks of developing monogenic (single-gene)
diseases. These are pathologies caused by mutations in only one gene. Such diseases include
cystic fibrosis, Fanconi anemia, sensorineural hearing loss, and a number of other conditions. As a rule, these diseases are either incurable or only partially correctable. Carriers of these genetic mutations often transmit monogenic diseases to their children and, consequently, to subsequent generations.
A history of recurrent non-viability at various stages
of gestation, including spontaneous miscarriages.
Inability to achieve natural conception due to impaired spermatogenesis or other pathologies, including cases of unexplained infertility.
The woman's age is over 35 years. Patients in advanced
reproductive age face an increased risk of unsuccessful IVF cycles.
Unsuccessful implantation or embryogenesis arrest in past IVF protocols, despite meticulous embryo selection.
Known severe hereditary conditions that are transmitted from generation to generation within the family.
The presence of chromosomal abnormalities in one of the partners or in immediate family members. Anomalies may manifest across generations, placing individuals at risk even if genetic irregularities occurred in distant relatives (grandparents, great-grandparents).
Women over the age of 35
Couples who have experienced recurrent miscarriages
Patients who have had several unsuccessful IVF treatments
Individuals with a family history or a previous child born with genetic anomalies
Cases involving low sperm quality or severe male factor infertility
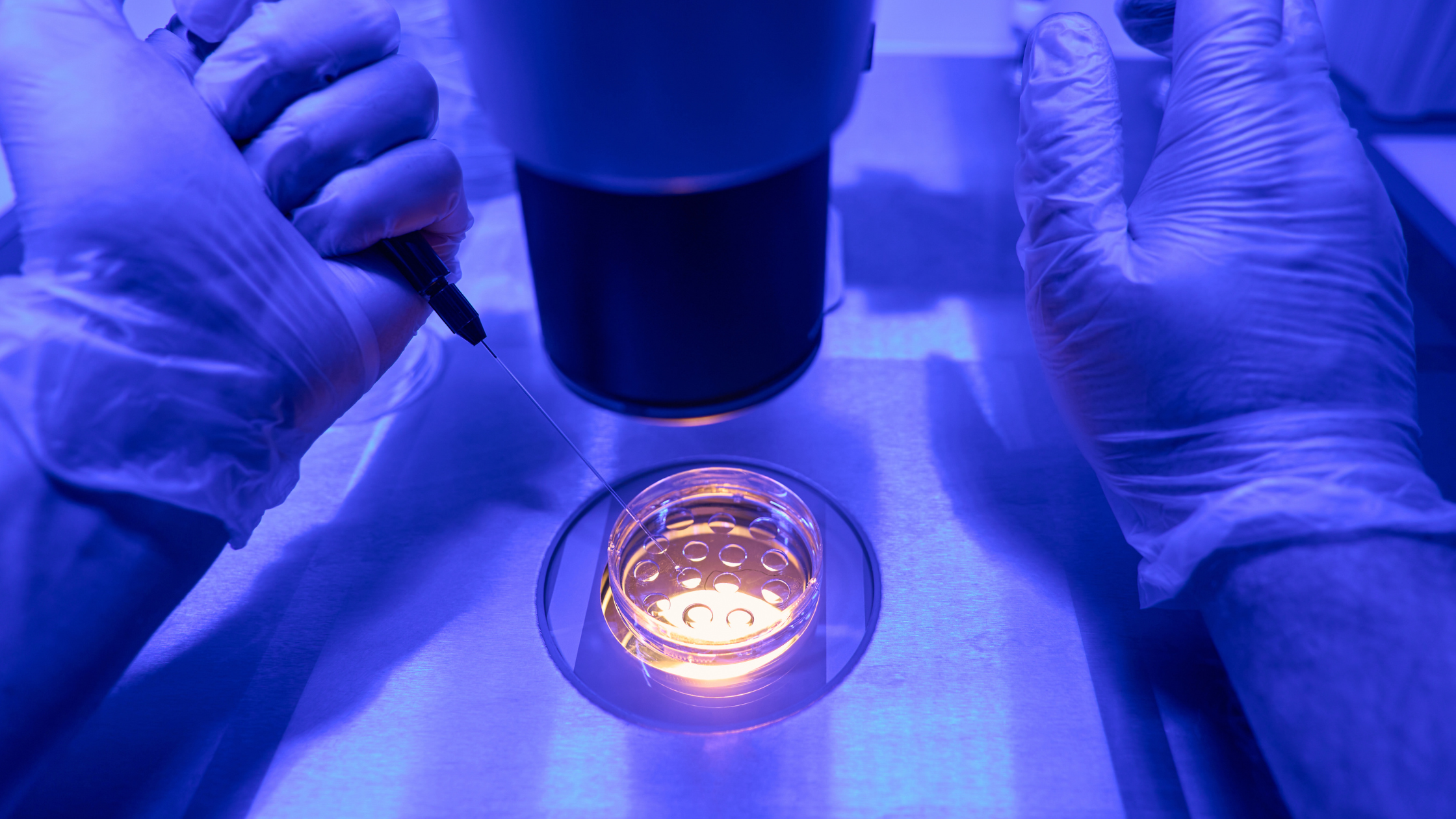
1. Embryo Biopsy
This is a microsurgical procedure carried out by the embryologist in the laboratory: Timing: It is typically performed on Day 5 or Day 6 of embryonic development, when the embryo reaches the blastocyst stage. Manipulation: Using micro-instruments, the embryologist samples 4–7 cells from the trophectoderm (the outer layer that will eventually form the placenta), without affecting the inner cell mass from which the fetus itself develops. Status: The biopsied embryo is usually subjected to cryopreservation (freezing) while awaiting the results of the genetic analysis.
2. Genetic Analysis
The biopsied material is sent to a genetics laboratory for DNA analysis: Objective: Geneticists determine the presence or absence of chromosomal anomalies (PGT-A), structural rearrangements (PGT-SR), or monogenic diseases (PGT-M). Result: The laboratory issues a report concluding the genetic status of each embryo. Based on this report, the doctor makes a decision regarding which of the genetically healthy embryos will be recommended for transfer into the woman's uterus.
Our clinic's location in the Famagusta (Gazimağusa), Glapsides region of Northern Cyprus puts you within easy reach of the area's best swimming beaches, restaurants, and resorts, allowing you to relax and unwind during your stay.
Located in Northern Cyprus, this is the most convenient option and is only a 40-minute drive from our clinic.
Located in the South of Cyprus, this is another popular option depending on your passport and flight availability.
To ensure your experience is completely stress-free from the moment you book your flights, your dedicated Patient Coordinator will manage all of your logistical arrangements. We handle every detail so you can focus on your treatment.
We will arrange for a driver to meet you upon arrival and transport you directly to your accommodation and appointments.
We can recommend and assist with booking your stay from a wide range of high-quality hotels, apartments, and boutique options that meet our standards for comfort and convenience.
From your arrival until your departure, we ensure every detail of your visit is thoughtfully managed.
Simply share your travel plans with your coordinator, and we will handle the rest.
For patients requiring an egg or sperm donor, we have a comprehensive and carefully managed donor programme. The process is governed by strict local regulations that ensure complete donor anonymity.
Our donors undergo rigorous screening, including extensive medical, genetic, and psychological evaluations, to ensure the highest standards of quality and safety. While the donor's identity remains anonymous, you will be provided with a detailed, non-identifying profile which typically includes:
This allows you to choose a donor with characteristics that are important to you while respecting the legal framework of anonymity.
We specialize in making the process seamless for our international patients. Your journey is managed by a dedicated International Patient Coordinator who will be your single point of contact.
After your initial consultation, we will create your bespoke treatment plan.
We offer two flexible pathways for our patients travelling from abroad.
For your convenience, you can begin the initial stages of your treatment at home. We will coordinate with a clinic in your home country for your preliminary scans and tests. You then travel to Cyprus to complete the final stages, requiring a stay of as little as one week for your key procedures. This option is popular as it minimizes your time away from home.
Alternatively, you can choose to undertake your entire treatment cycle with us in Cyprus. This allows you to step away from daily routines and relax in our calm, supportive environment. This all-inclusive pathway typically requires a stay of approximately three weeks.
Whichever pathway you choose, your coordinator will assist with planning your trip, providing recommendations for premium accommodation and organizing private airport transfers. Our goal is to manage all the logistics, allowing you to focus completely on your treatment in a calm, stress-free environment.
This is often the first and most important question we receive. While we are proud of our excellent success rates, which are in line with top European clinics, we believe in providing you with a transparent and realistic perspective. Rather than focusing on a single, generic statistic, we provide a personalized success projection during your initial consultation. This is based on your specific age, medical history, and diagnosis.
Our success is built upon the expertise of our world-class clinicians and embryologists, who utilize state-of-the-art laboratory technology. We are committed to ethical and transparent reporting, ensuring you have the confidence and clarity you need to make an informed decision.